
Most people are familiar with police officers’ use of “breathalyzers” to determine whether a motorist is legally considered to be driving under the influence of alcohol. Kevin Limtao, a lead systems engineer at Triple Ring Technologies in Boston, was first introduced to the field of breath analysis when working on a roadside screening system for other drugs of abuse.
For his capstone Systems Engineering project, he developed a Breath Analysis System for use by physicians and clinicians to diagnose respiratory viruses and bacteria.
What problem were you trying to solve or what question were you trying to answer?
Breathalyzers detect alcohol, but many drugs of abuse are non-volatile and cannot be detected this way. Instead, you need to look at respiratory droplets.
Historically, breath analysis has focused on gases or volatile compounds, with tests for conditions like Helicobacter pylori and asthma. There is considerably less attention paid to markers carried in respiratory droplets, because of the large variance in respiratory droplet emissions across different people and environments. Another reason is a lack of predicate devices that use breath as a sample type. A system that can control for variance in respiratory droplet emission can provide diagnostic opportunities not currently available.
My system aims to bridge these gaps with a breath collection front-end that consistently collects respiratory droplets for use in established diagnostic assays detecting respiratory pathogens. The goal is to provide precedence for a breath analysis system that can enable future diagnostic applications.
How did you use Systems Engineering to tackle this task?
Several systems engineering tools were useful in conceptualizing this system. A needs analysis was critical, exploring diagnostic limitations and breath’s potential via stakeholder interviews. The initial concept differed from the final system design based on stakeholder feedback about needs and problems a breath analysis system must address.
Functional analysis and iterative decomposition were necessary to determine breath collection subsystem functions like controlling humidity and flow to maintain droplet sizes for consistent collection efficiency. These performance requirements need definition early in development.
Trade studies evaluated commercial diagnostic panels’ sensitivity/specificity tradeoffs relative to turnaround time and cost. Integrating these assays leverages established technologies to enhance system capabilities.
The iterative nature of Systems Engineering enabled continuous refinement based on insights throughout development.
What did you create to solve this problem?
The focus was generating a conceptual design, including the breath collection subsystem, a trade study to select a pathogen detection device, and the identification of interfaces. Systems engineering artifacts like a Functional Analysis, Conceptual Design Report, and System Specification provide a detailed roadmap for subsequent development.
The design represents a structured approach to respiratory pathogen diagnosis from breath, outlining technical aspects and integration into clinical workflows to emphasize the broader healthcare impact.
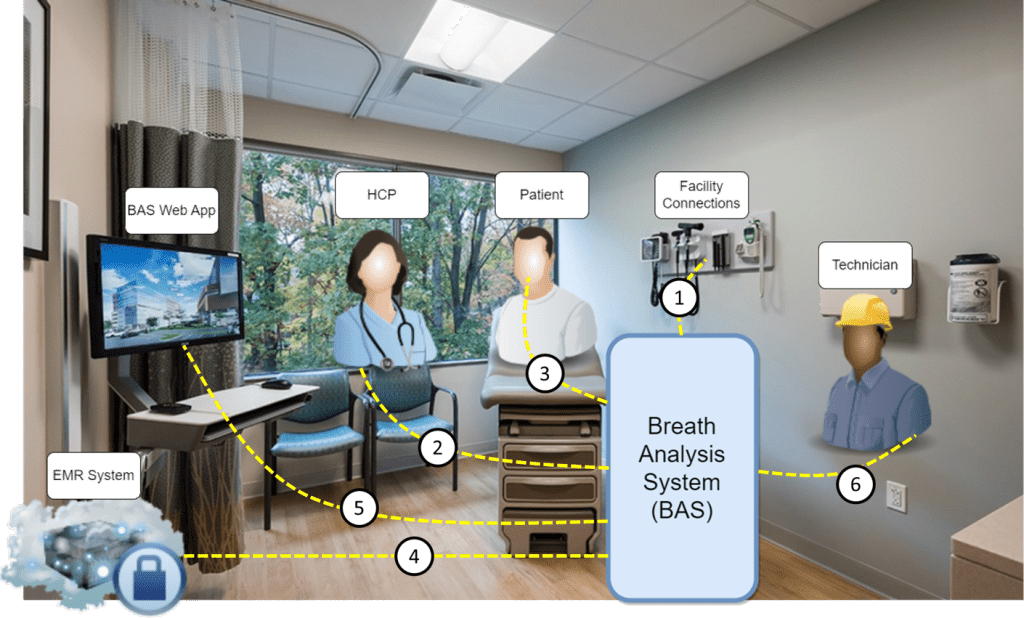
Kevin Limtao’s visualization of the Breath Analysis System in a healthcare setting.
What are the potential practical ramifications and uses?
Non-invasive diagnostics using breath, sweat, or saliva is not a novel goal. Diagnosis or prognosis of disease states using breath, sweat, or saliva has been a holy grail for medical device manufacturers for many years. For any sample matrix, it is vital to understand how well the sample can be used to represent the disease state or condition. If we look at other sampling means such as nasopharyngeal swabs, we know it is possible to sample airway lining fluid in the upper respiratory tract. However, sampling of the lower respiratory tract is currently limited to more invasive procedures such as bronchoalveolar lavage.
My system aims to provide lower respiratory tract sampling to enable respiratory pathogen detection. This could potentially replace procedures like bronchoalveolar lavage for conditions like Pneumocystis pneumonia.
Until consistent respiratory droplet collection is validated, breath analysis will be limited. If achieved, breath could replace less sensitive/specific sample types for many indications. Integrating advanced molecular testing with improved breath droplet analysis techniques can enable further diagnostic platforms.
What’s next for this project?
I hope to continue breath analysis work and apply learnings to developing complex in vitro diagnostic systems. I am thankful that JHU has provided me with a skill set that is broadly transferrable to other applications as well.
Anything else you want to tell us?
My current role at Triple Ring has given me a unique opportunity to work on a myriad of early-stage in vitro diagnostic systems and I could not be more grateful. My wife and I are currently based out of Boston, and I have her to thank for providing a critical eye on my system design due to her experience as a pediatric critical care doctor.